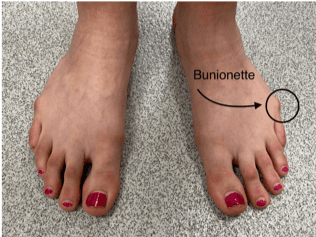
What is an Bunionette?
This uncommon condition causes a prominent swelling and bump at the base and outside of the little toe.
What are the symptoms of Bunionette?
The main concern is excessive rubbing and redness associated with the bump. As the bunionette gets bigger it can rub more, causing pain, hard skin and blistering, as well as difficulties getting shoes to fit. It usually starts to cause problems after the age of 10 years.
What causes this?
The shape of the long toe (metatarsal) causes the bump. We do not know exactly what causes bunionette but it can affect several generations of the same family, which implies that it is sometimes passed on from parent to child (inherited).
What is the natural history of this condition?
If the foot remains asymptomatic (no symptoms) and pain free, we tend to observe and leave well alone. We would encourage moisturisation with cream after baths and wide fitting shoes for comfort.
How can it be treated?
Treatment options are quite binary.
Option A. Leave alone and observe: we tend to do this in asymptomatic or patients who present younger than their teenage years
Option B. Surgery to straighten the toe: the operation is done under a general anaesthetic as a day case procedure. At the time of consent, we would discuss the procedure in detail with you, including the benefits and the risks of the surgery, as well as the post-operative care. Please see the separate information leaflet regarding surgery.
Bunionette Surgery
What does the operation involve?
The operation is done under a general anaesthetic as a day case procedure. We also numb the toe with local anaesthetic. It is quite a big operation through a medium sized scar along the side of the toe. The bump is shaved off and the bone is cut and reset in a much straighter position. It is held with tiny orthopaedic screws. This is done under X ray control during the surgery. Dissolvable stitches are used as well as paper stitches and a big wool and crepe dressing is applied.
What is the aftercare?
It is extremely important to elevate the foot for 72 hours after the operation. This helps the swelling settle and aid healing. A temporary splint (half plaster) is used with a heel-walking shoe. Crutches are useful to get around, but not essential, particularly at school. Patients are seen in clinic around 2 weeks after the operation to check the scar is healing, to redress the wound and to obtain an x ray. Most patients would slowly wean into a shoe with a nice wide toe box at this stage. Return to sports and activities is allowed after a final check and x ray at about 8 weeks.
What are the success rates?
The vast majority of families are very happy with the result. There is always a small chance of problems, but this is rare.
What are the risks of surgery?
The risks of surgery are small and include the general surgical risks of any surgery. These include infection, ugly scar, skin numbness. More specific risks of this operation include fracture recurrent deformity and tendon damage. These risks will be discussed in detail with you before we proceed.
