What is the tibial tubercle?
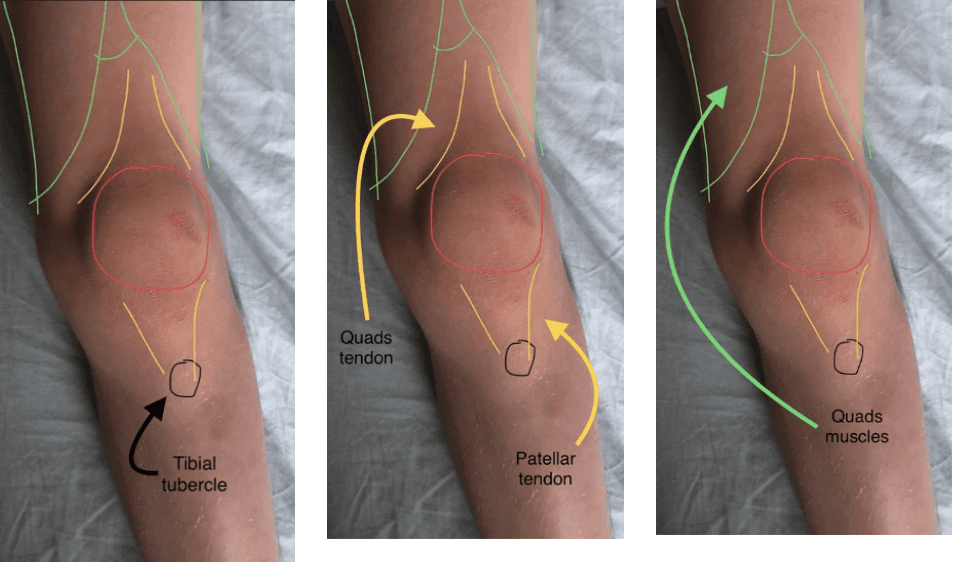
This is the bony lump at the top and front of the shin bone (tibia). It is where the kneecap (patellar) tendon attaches to the bone, which is the insertion point of the extensor mechanism of the knee.
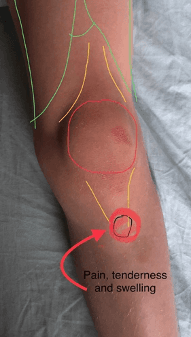
Pictures 1, 2 and 3 – Child’s knee
What is the extensor mechanism of the knee?
This comprises of the 4 quadriceps muscle of the thigh, the quads tendon above the knee cap (patella), the knee cap itself and the patellar tendon, which inserts into the tibial tubercle at the top end of the shin bone (tibia). As these muscles contract the knee straightens. (extends)
What is an apophysis?
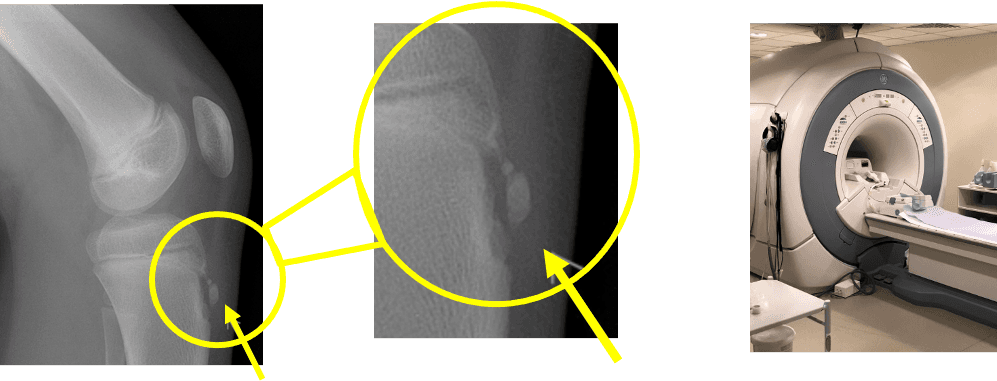
An apophysis is a skeletal growth area under a tension or pulling force. The largest apophysis in the lower leg is at the tibial tubercle. (see picture 4)
Picture 4 – Lateral X Ray of child’s knee with close up of tibial apophysis. Picture 5 – MRI scanner.
What is apophysitis?
When the bony lump and its soft tissue covering becomes swollen and red this inflammation is termed apophysitis.
(see Picture 5)