UKR – Partial (Unicompartmental) Knee Replacement
Nev Davies – Consultant Knee Surgeon
Reading Hip & Knee Unit
Patient Information Leaflet
Introduction
This guide has been written to help you gain a better understanding about a partial or unicompartmental knee replacement (UKR) and what is involved before, during & after the operation.
We know from experience that the more information the patient can acquire about the process the better the outcome is likely to be.
A UKR is a major surgery and the decision to have one needs to be balanced and thought through carefully. It is extremely important to make sure you have exhausted non-operative management options for your knee problem. It is also essential that you understand that the operation is only half the treatment and the period of physiotherapy and rehabilitation after surgery is vitally important for a good outcome.
What is a Partial (Unicompartmental) Knee Replacement (UKR) ?
A UKR is an operation that involves replacing the surface of one compartment of a damaged knee joint with a specialised metal and plastic implant.
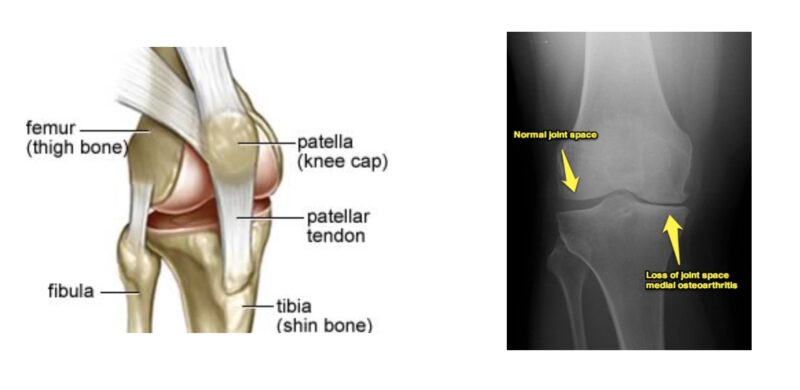
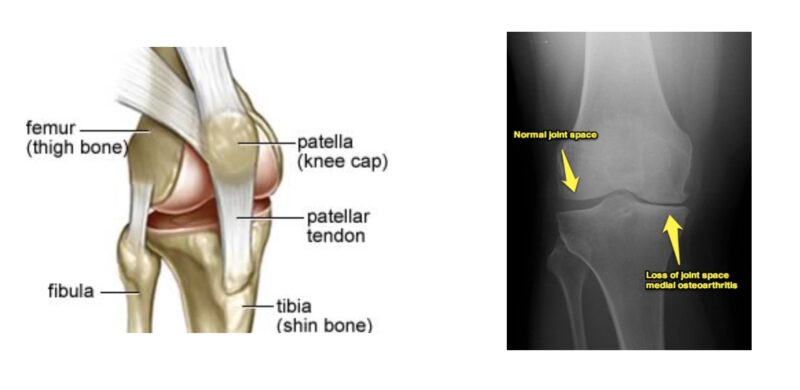
The ‘main’ knee joint is made up of the articulation between the thigh bone (femur) and the shin bone (tibia). The kneecap (patella) glides up and down a groove on the front of thigh bone (femur) as we bend and straighten the knee. The most common form of damage to the joint is the result of degenerative osteoarthritis or ‘wear and tear’. This is the result of thinning and eventually absence of the smooth articular cartilage that covers the end of each bone to make up the joint surface. This roughening and distortion of the joint surface causes pain and stiffness. Patterns of wear within a knee follow a predictable course. In a significant number of arthritic patients only the inside of the joint wears out which makes a partial knee replacement an option as opposed to a full total knee replacement.
What are the benefits of UKR ?
The ‘new joint’ is primarily recommended for pain relief, but it also serves to restore pain free movement, correct deformity and consequently improved walking and activity.


What are the alternatives to UKR ?
Patients with arthritis tend to take a mixed course with periods of pain and flare ups, mixed with good spells. Patients who decide to have partial knee replacement should have explored and exhausted all the other non-operative treatment modalities before opting for surgery. These include:
- Regular painkillers. Paracetamol and anti-inflammatories such as ibuprofen can help control the pain. Supplements to your diet may also help relieve your symptoms. You should check with your doctor before you take supplements.
- Physiotherapy to strengthen the lower leg muscles is so important and cannot be emphasized enough.
- If overweight, a concerted effort to lose some weight will take pressure off the knees when standing and walking.
- Using a walking stick or wearing an elasticated knee support can support your knee and make walking easier. Regular moderate exercise will help to reduce stiffness in your knee.
- Using a special knee brace called an ‘offloader brace’ can sometimes help for specific patients.
- A steroid injection into your knee joint can sometimes reduce pain and stiffness but the duration of relief is often variable and depends on the extent of osteoarthritis present. Other injection therapies are available but there is no good research evidence to say they are any better than a steroid injection.
- A keyhole operation (arthroscopy) is sometimes offered if you are having mechanical symptoms, (catching, locking or giving out) to clean out the knee joint. This can give some relief, but it is usually temporary. It is certainly not offered as a routine option.
- Unfortunately, as arthritis tends to deteriorate over time and get worse, all these measures become less effective, leaving knee replacement as the last definitive intervention.
Partial vs Total Knee Replacement
An MRI scan is obtained for patients to confirm that just the inside of the joint is damaged and the important stabilising cruciate ligaments are intact. If there is significant arthritis in the knee cap or the outside joint compartment, then a total knee replacement is a better option. I am happy to discuss this further with you at any point.
Expectation – How successful is a Partial Knee Replacement ?
I tell all our patients that on average, 90% of people(18 out of 20 patients) are absolutely delighted with the result of the surgery. Their pain is significantly better, and their walking is much improved.
About 5% of people (1 in 20 people) are unlucky and have some kind of complication or side effect secondary to the surgery. As with all operations there are risks involved. Some of these complications are small and can be rectified easily, some are more serious and require closer monitoring and further intervention. There is a separate section on risk later in this leaflet. We will also go through these possible complications and risks in more detail with you during the consent process.
A further 5% of people (1 in 20) are left with something they did not expect from the surgery, although their arthritic ‘bone-on-bone’ pain has usually gone. This could be an on-going ache, a different pain, a niggle, a numbness or a stiffness that they were not expecting before they underwent the surgery, and so are not as happy as they thought they would be. The only way we can explain this to patients is that we are not giving you your native knee back but replacing the damaged knee with specialised metal and plastic implants. The important thing to note in this group of patients is that you may continue to improve up to 18 months to 2 years after surgery. It is essential to work hard with post-operative exercises and physiotherapy to strengthen things up as best as possible. I have a knee replacement agreement form that I encourage patients to read and sign before we go ahead.
Having said all this, it must be reiterated that the vast majority of patients are delighted with this surgery which is successful and really helps improve their quality of life.
What happens in hospital?
The day of admission
Patients are admitted on the day of surgery and are seen by the anaesthetist to discuss the different types of anaesthetic involved and by myself to answer any final questions, go through the final consent process and mark the correct leg.
Risks and potential complications of UKR
Common (2-5%)
- Pain
Pain is to be expected following every type of surgery. The post op surgical pain is worst in the first few days but then starts to settle. You will be given medication to control the pain both post operatively and on discharge. - Bleeding & Bruising
This can happen during or after surgery and there is a possibility (rare) that this may require a blood transfusion. - Blood clots (Deep Vein Thrombosis)
These usually occur in the legs (DVT) and can very occasionally move through the blood stream to the lungs (pulmonary embolus) making it difficult to breath. A pulmonary embolism may be fatal (3 in 1000 cases). The risk of forming such clots is greater after any surgery especially lower limb surgery. You will be given treatment in advance to reduce the risk of blood clots forming. Starting to walk and moving early is one of the best ways to prevent blood clots from forming. - Difficulty passing urine (males especially)
If this persists you may be given a bladder catheter (tube) until you are more mobile. - Progression of Arthritis
The wear may progress to the outside of the joint or the knee cap joint and ultimately a total knee replacement maybe required.
Less common (1-2%)
- Infection of the surgical wound
You will be given a large dose of antibiotics just before your surgery and the procedure is performed in a clean environment (theatre) with sterile equipment. Despite this, infections still occur. The wound may become red, hot and painful (infected). This usually settles with antibiotics but may require an operation to wash out the joint if there are concerns that the metalwork is involved (deep infection). Very, very occasionally the metalwork may need to be removed and replaced at a later stage. - Dislocated bearing
The small, specialised plastic insert that fits in the new joint can ‘pop’ out of joint and the knee becomes locked. In this instance patients require an operation to remove the bearing and insert a new one. - Knee stiffness
Stiffness may be a problem especially if the movements were significantly restricted pre-operatively. At 6 weeks if your bend is not as good as it should be, a manipulation (under anaesthetic) may be necessary.
Rare (<1%)
- Damage to the nerves around the knee
Efforts are made to avoid this. However, damage to the small skin nerves can result in some temporary or permanent alteration of sensation to the skin on the front of the knee. Rarely the larger nerves around the knee can be involved and this can result in temporary or permanent weakness and/or altered sensation in the lower leg or foot. - Prosthesis wear and loosening
Modern techniques and implants mean about 80% of knee replacements will last over 15 years. If early loosening does occur this most likely will require further surgery. - Damage to the blood vessels behind the knee
This can lead to loss of circulation to the leg and foot. If this happens you will need immediate surgery to restore the blood flow and could (very rarely) result in amputation. (PS: I have never seen this) - Bumpy Scar
Most wounds heal well but sometimes scars can ‘over heal’ causing a keloid.The operation takes between 1-2 hrs but afterwards patients spend some time in recovery (an area in theatre where monitoring of blood pressure and breathing takes place) before you return to the ward.
After surgery
Exercises
Once back on the ward you will be encouraged to move around as much as comfort allows. You should move your feet and ankles, and your operated knee within the limits of the bandaging. Apart from moving your operated leg you should also try and move around in bed to avoid pressure areas on your bottom and heels, and it is advised to practice deep breathing exercises to encourage good lung function.
Eating and Drinking
Following your operation, you may feel sick which is a common symptom following surgery and a side effect of pain-relieving drugs. Once you can tolerate fluids you will be started on a light diet, increasing to a full diet within 48 –72 hours. If nausea is a continuing problem, there is medication available which can minimise it in most circumstances.
Wound
At the end of your operation the incision over the front of your knee will be closed with stitches inside and surgical clips. The dressing we apply in theatre is left in place unless there is significant bleeding under the dressing. This minimises the risk of contamination and possible wound infection. Clips will need to be removed 10-14 days after your operation. These can be removed either by myself in clinic or at your local surgery by the GP nurse. You will be able to shower whilst the clips are still in.
Pain relief
Pain relief after your operation can be kept to acceptable levels by a variety of medications and techniques. Your anaesthetist who will have chosen the most suitable pain relief medication for your needs will have prescribed these. Your pain level may be acceptable while resting but may increase when you move. Therefore, it may be advisable to ask for a “top-up” 10 to 15 minutes before physiotherapy treatment. Ice packs and / or cooling bandages placed on the knee are also beneficial for pain relief and swelling. Your physiotherapist or nurse can help you with this. A compression cryocuff (ice duvet) is available to hire post operatively and information can be found here.
Swelling
It is normal to expect swelling and bruising of your knee, leg and foot following this surgery. This can take several months or more to resolve. However, if you notice a sudden increase in the swelling with pain and redness of the skin please contact the hospital or your G.P.
Physiotherapy
Normally patients who have had a knee replacement are independently mobile, getting in and out of chairs, getting in and out of bed and walking around the ward within a few days. The physiotherapists will help you get up and walking from day 1, and undertake the exercises needed.
On discharge from hospital
On discharge a letter will be sent by the hospital to your GP which summarises what operation and treatment you have received, but this often takes a few days before it arrives. Your wound will be covered by a dressing and underneath this the metal clips will need to be removed either by myself in clinic or by your GP nurse at around 10 days post op. You will be further reviewed by myself in the outpatient clinic at 6-8 weeks for a check-up and an X-ray. The average hospital stay for a partial knee replacement patient is 2 to 3 days, but it can vary between individuals.
How mobile will I be after discharge?
Before you can leave the hospital, you should be independently mobile with your crutches and be safe walking up and down stairs. You will still be encouraged to put as much weight through your operated leg as possible.
Although you will be encouraged to get outdoors for short periods, for most of the first six weeks you will be indoors and should travel outdoors preferably with a friend or family member.
When can I drive?
Normally patients are advised to refrain from driving for at least six weeks, i.e. until clinic review. If the operated leg is your right knee it is often harder to recover sufficiently to allow safe operation of the brake and it could be 10 weeks or so before you are safe to drive. As a general rule, once you are able to walk without crutches or sticks without a limp, you are able to drive.
When can I return to work?
Most patients will be off work for around three months. If your work is sedentary or supervisory you can return to work in a part time capacity or on light duties from six weeks post-surgery, but this would only be if you have a degree of control over your working environment. Normally return to work will be discussed more formally at the clinic visit.
What medication will I need following discharge?
You will be given the medication which you brought into hospital and if you are on medication for other medical conditions such as diabetes, asthma or blood pressure treatments, these should be continued on leaving hospital. Specifically, regarding the knee operation you may require a few weeks supply of analgesics such as paracetamol or anti-inflammatories such as ibuprofen. You will also be given a tablet (Rivaroxaban) for 10 days post operatively which thins the blood and reduces the risk of developing deep vein thrombosis (DVT).
What exercise should I do?
Prior to discharge from hospital you will have been seen by the physiotherapists and given an exercise programme to follow. This is important firstly to get your knee working properly following the operation and secondly to help recover any muscle loss which has occurred as a result of your arthritis. Usually the physiotherapist will arrange for you to be reviewed as an outpatient. On average this would be once per week during the first few weeks following discharge. This will allow the physiotherapists to monitor progress and give further advice and encouragement as required. The amount of physiotherapy will be dependent on individual circumstances.
Long term care
Health and general fitness are important. We would advise that you try to keep your weight down, thereby reducing the stress on the knee joint.
The risk of infection after your knee replacement is extremely low. However, as a precaution please notify your G.P. if you get any kind of infection, so that you can receive antibiotics as soon as possible. In addition, you must inform your dentist of your joint replacement.
The Other Knee
If your other knee is also arthritic there will come a time when it becomes more painful and you may choose also to have this replaced. A safe time in between operations is about 3 months.
If you have any questions, please don’t hesitate to contact us!








