Osgood-Schlatter’s Condition
Osgood-Schlatter’s Condition (Tibial Tubercle Apophysitis)
This blog aims to explain the functional anatomy, clinical symptoms and treatment plan for patients presenting with this common growth related anterior knee pain.
What is the tibial tubercle?
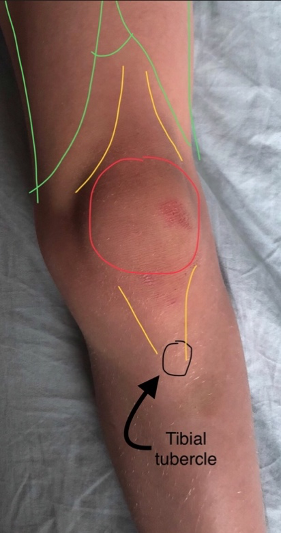
This is the bony lump at the top and front of the shin bone (tibia). It is where the kneecap (patellar) tendon attaches to the bone, which is the insertion point of the extensor mechanism of the knee.
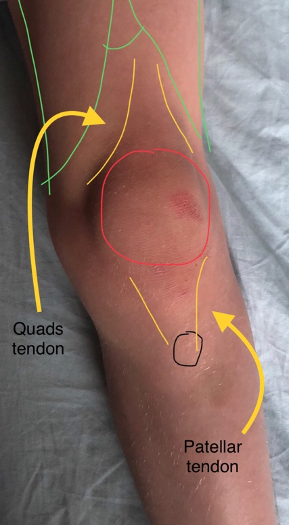
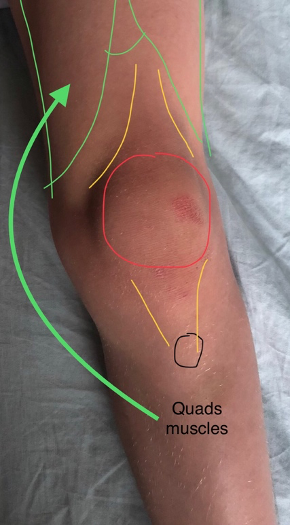
Pictures 1, 2 and 3 – Child’s knee
What is the extensor mechanism of the knee?
This comprises of the 4 quadriceps muscle of the thigh, the quads tendon above the knee cap (patella), the knee cap itself and the patellar tendon, which inserts into the tibial tubercle at the top end of the shin bone (tibia). As these muscles contract the knee straightens. (extends)
What is an apophysis?
An apophysis is a skeletal growth area under a tension or pulling force. The largest apophysis in the lower leg is at the tibial tubercle. (see picture 4)
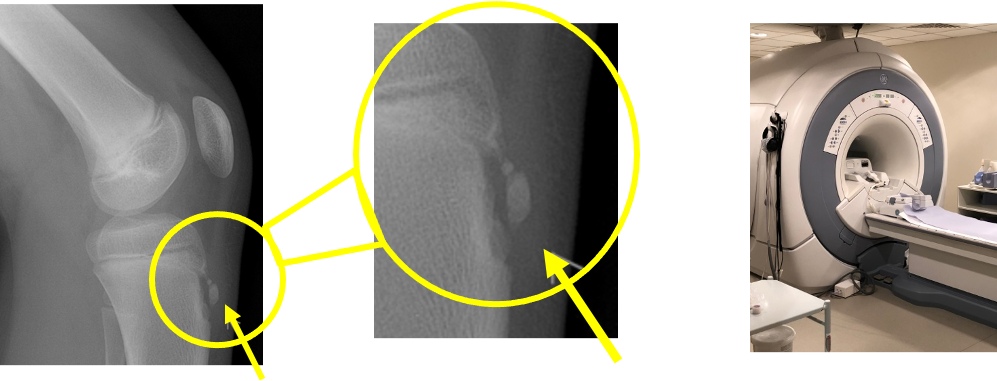
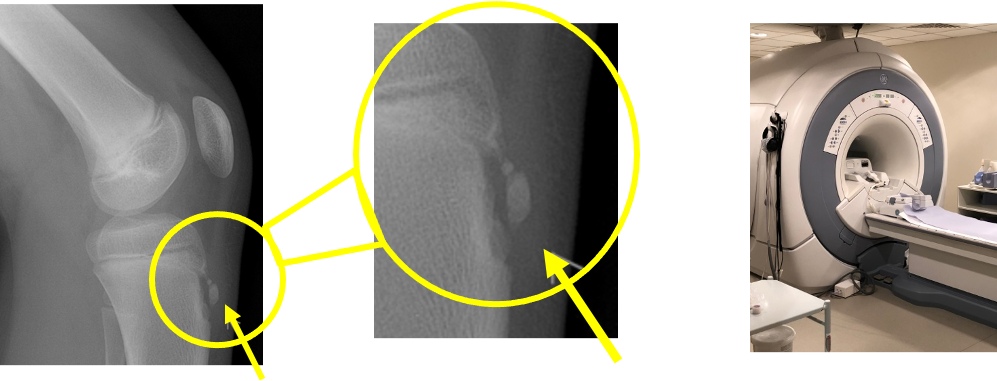
Picture 4 – Lateral X Ray of child’s knee with close up of tibial apophysis. Picture 5 – MRI scanner.
What is apophysitis?
When the bony lump and its soft tissue covering becomes swollen and red this inflammation is termed apophysitis.
(see Picture 5)
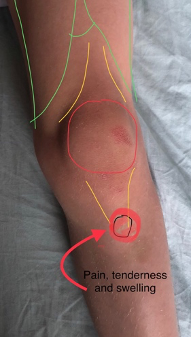
Picture 6 – Child’s knee with location of tender spot.
Why does it happen?
The repetitive tension (pulling) force of the tendon inflames the growth area during activity particularly jumping sports, such as football and netball. This is particularly troublesome at times of skeletal bone growth (growth spurts).
Who gets it?
It affects active boys and girls at times of skeletal growth. This typically, but not exclusively, occurs between the ages of 8 and 12 years. It is fairly common, affecting approximately 1 in 5 children of this age.
What are the clinical symptoms and signs?
It is characterised by pain and/or a tender lump at the front of the shin bone, just below the kneecap. (see picture 6)
The pain varies from person to person. Some have only mild pain while performing certain activities, especially running and jumping. For others, the pain is nearly constant and debilitating. It usually occurs in just one knee, but sometimes it develops in both knees. The discomfort can last from a few weeks to many months and may recur until your child has stopped growing.
How is it diagnosed?
Osgood Schlatter’s condition is usually diagnosed clinically ie: after talking a history and examining the knee, however X-rays (see Picture 4) and occasionally MRI scans (see Picture 5) are used to rule out any other problems with the knee joint itself.
What is the treatment?
Treatment is always non-operative and involves a number of strategies:
1. Avoiding the specific activities that really aggravate the pain.
1. Education and reassurance that the pain experienced is not serious and that things improve after growth stops.
3. Simple anti-inflammatories (ibuprofen) and simple painkillers (paracetamol).
2. Ice packs applied (wrapped in a cover) when the area is inflamed, after sports.
4. Physiotherapy and exercises to stretch out tight muscles and tendons.
5. Very occasionally we advise crutches or a walking plaster to allow a period of rest.